Uterine fibroids, also known as fibroids or leiomyomas, are non-cancerous growths that develop in or around the uterus. They are one of the most common gynecological conditions, affecting nearly 60–70% of women by the age of 50. While many fibroids are asymptomatic, others can significantly affect a woman’s quality of life.
This comprehensive guide explains everything you need to know about uterine fibroids—their causes, symptoms, types, diagnosis, treatment options, and when to seek medical care.
What Are Uterine Fibroids?
Uterine fibroids are benign tumors composed of smooth muscle cells and fibrous connective tissue. They vary in size—from as small as a seed to as large as a melon—and may occur singly or in clusters.
Fibroids are not cancerous and do not increase the risk of uterine cancer. However, their location and size can cause significant symptoms.
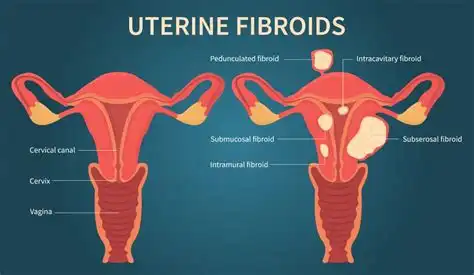
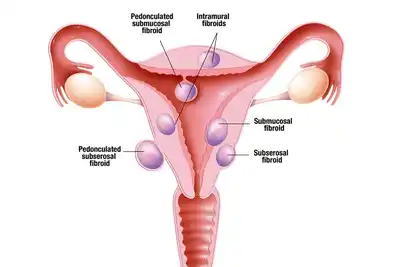
Types of Uterine Fibroids
- Intramural fibroids – Grow within the muscular wall of the uterus
- Subserosal fibroids – Project outside the uterus
- Submucosal fibroids – Grow into the uterine cavity (most symptomatic)
- Pedunculated fibroids – Attached to the uterus by a stalk
Causes and Risk Factors of Uterine Fibroids
The exact cause of uterine fibroids is unknown, but several factors contribute to their development:
- Hormonal imbalance (estrogen and progesterone)
- Family history of fibroids
- Early onset of menstruation
- Obesity and vitamin D deficiency
- Nulliparity (not having given birth)
Common Symptoms of Uterine Fibroids
Many women with fibroids experience no symptoms. When symptoms occur, they may include:
- Heavy or prolonged menstrual bleeding
- Menstrual periods lasting more than 7 days
- Pelvic pain or pressure
- Lower back pain
- Frequent urination or difficulty emptying the bladder
- Constipation
- Pain during intercourse
- Infertility or recurrent pregnancy loss
How Are Uterine Fibroids Diagnosed?
Fibroids are often detected during a routine pelvic examination. To confirm the diagnosis, the following investigations may be used:
- Pelvic ultrasound (transabdominal or transvaginal)
- MRI pelvis for detailed mapping
- Hysteroscopy for submucosal fibroids
- Saline infusion sonography
Treatment Options for Uterine Fibroids
Treatment depends on the size, number, symptoms, age, and fertility plans of the patient.
1. Conservative Management
- Observation and regular follow-up
- Pain relief medications
2. Medical Treatment
- Hormonal therapy
- GnRH analogues
- Progesterone modulators
3. Minimally Invasive Procedures
- Hysteroscopic myomectomy
- Laparoscopic myomectomy
- Uterine artery embolization (UAE)
4. Surgical Treatment
- Myomectomy (uterus-preserving)
- Hysterectomy (definitive treatment)
Uterine Fibroids and Pregnancy
Most women with fibroids can conceive naturally. However, fibroids—especially submucosal ones—may cause infertility, miscarriage, preterm labor, or malpresentation.
Read more about pregnancy-related complications.
When Should You See a Gynecologist?
You should consult a gynecologist if you experience:
- Heavy bleeding causing anemia
- Severe pelvic pain
- Rapid increase in fibroid size
- Difficulty conceiving
Authoritative Video on Uterine Fibroids
Watch this trusted medical video explaining fibroids clearly:
Uterine Fibroids Explained – Mayo Clinic
FAQs on Uterine Fibroids
Are uterine fibroids dangerous?
Fibroids are usually benign but can cause significant symptoms if untreated.
Can fibroids shrink naturally?
Fibroids may shrink after menopause due to reduced estrogen levels.
Do fibroids turn into cancer?
Malignant transformation is extremely rare (<1%).
Can fibroids cause infertility?
Yes, especially submucosal fibroids that distort the uterine cavity.
Is surgery always required?
No. Many fibroids can be managed conservatively or medically.
Trusted External References
- Mayo Clinic – Uterine Fibroids
- American College of Obstetricians and Gynecologists (ACOG)
- World Health Organization (WHO)
Conclusion: Uterine fibroids are common and manageable. Early diagnosis and individualized treatment can greatly improve quality of life and reproductive outcomes.